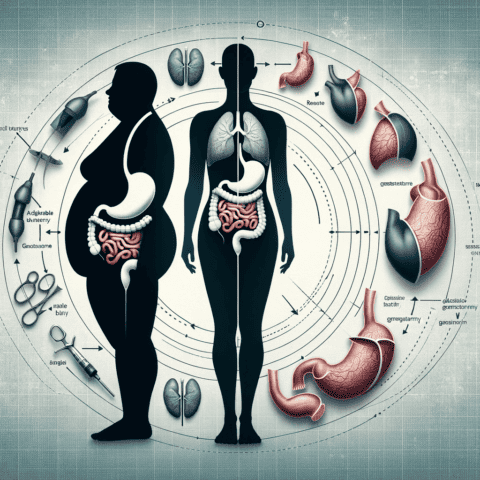
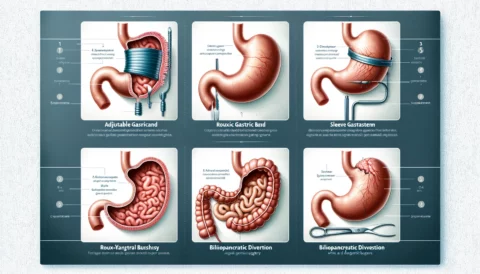
Weight loss surgery leads to dramatic changes in a person’s physiology and nutritional needs. Procedures like gastric bypass and sleeve gastrectomy reduce the size of the stomach and change how food is absorbed in the intestines. This helps patients lose a significant amount of weight, but it also impacts how their body gets essential vitamins and minerals from food.
After bariatric surgery, patients have to follow strict vitamin and mineral supplementation protocols to avoid potentially dangerous nutritional deficiencies. Dallas bariatric surgery center Peak Bariatric Surgery provides patients with comprehensive guidelines on vitamins and minerals after weight loss surgery. Their expert medical team recognizes the importance of this aspect of aftercare.
Why Nutritional Deficiencies Occur After Bariatric Surgery
Weight loss surgery decreases the amount of food a person can eat at one time and reduces absorption of nutrients. This inevitably leads to some vitamin and mineral deficiencies if supplementation is not started promptly after surgery.
Some of the main reasons nutritional deficiencies occur include:
- Decreased stomach size – The smaller stomach pouch created by gastric sleeve and gastric bypass limits food intake, which reduces vitamin and mineral consumption.
- Bypassing parts of the digestive tract – Gastric bypass in particular bypasses parts of the stomach and small intestine that absorb nutrients like iron, calcium, and vitamin B12.
- Nausea and vomiting – Some patients experience nausea and vomiting after surgery, which inhibits intake and absorption of vitamins and minerals.
- Dumping syndrome – This common side effect causes food to “dump” rapidly into the small intestine, resulting in diarrhea and preventing optimal absorption.
- Changes in appetite and food preferences – Patients often avoid vitamin-rich foods like meat, greens, and dairy after surgery.
- Non-compliance – Some patients may neglect to take their prescribed supplements regularly.
Without supplementation, nutritional deficiencies can develop within the first 1-2 years after surgery. Ongoing supplementation and monitoring are necessary to protect long-term health.
Key Vitamins and Minerals to Supplement After Bariatric Surgery
The ASMBS guidelines outline the essential vitamins and minerals that bariatric patients need to supplement post-surgery:
Multivitamin with Minerals
A complete multivitamin containing at least 18 mg iron, 400 mcg folic acid, and 200% of Recommended Daily Intake for other vitamins and minerals. Two multivitamins per day are often recommended.
Vitamin B12
Vitamin B12 deficiency is common after weight loss surgery since it is primarily absorbed in the bypassed parts of the stomach. Intramuscular B12 injections or high-dose oral supplements (1,000-2,000 mcg daily) are prescribed.
Calcium Citrate
Calcium citrate is recommended over calcium carbonate for better absorption. 1,200-1,500 mg calcium daily is advised.
Vitamin D
2,000-3,000 IU of Vitamin D (often in the multivitamin) is recommended for bone health.
Iron
45-60 mg elemental iron may be prescribed, often as iron polysaccharide which is better absorbed.
Other Vitamins and Minerals
Zinc, copper, selenium, thiamine, vitamin A, and vitamin K supplementation may be prescribed on an individual basis.
In some cases, additional B complex vitamins, magnesium, and vitamin C are recommended if deficiencies occur.
Importance of Lifelong Supplementation After Bariatric Surgery
Metabolic changes from weight loss surgery make vitamin and mineral supplementation a lifelong necessity for optimal health. Deficiencies can develop months or years after surgery if supplementation stops.
Potential consequences of nutritional deficiencies include:
- Fatigue, weakness, and headaches
- Hair loss and skin changes
- Poor wound healing
- Anemia
- Neuropathy
- Bone fractures
- Seizures
- Visual problems
- Impaired immunity
By adhering to the recommended vitamin and mineral protocols, most deficiencies can be avoided. However, regular monitoring of vitamin levels through lab work is still important to catch potential issues early.
Dallas bariatric surgery centers like Peak Bariatric Surgery provide long-term nutritional counseling and follow-up to ensure patients continue meeting their needs safely after surgery. Close monitoring and patient education help minimize risks and support the best possible health outcomes long-term.
Key Takeaways: Vitamin and Mineral Supplementation After Bariatric Surgery
- Weight loss surgery reduces absorption and intake of vitamins and minerals, increasing risk of deficiencies.
- Lifelong supplementation with a multivitamin, calcium, iron, vitamin B12, vitamin D, and other nutrients is necessary.
- Regular lab work monitors for potential deficiencies requiring additional supplementation.
- By following nutritional protocols, patients can avoid complications and support good health long-term.
Thorough education and preparation for the lifelong vitamin and mineral regimen empowers bariatric surgery patients to protect their health. Dallas bariatric centers provide this nutritional counseling and follow-up care critical for success. With proper supplementation and monitoring, patients can safely manage their altered nutritional needs after weight loss surgery.
Preparing for a Lifetime of Vitamin Supplementation
Bariatric surgery patients must be prepared to adhere to vitamin and mineral protocols for life. Dallas bariatric surgery centers emphasize this during the pre-operative education process.
Here are some tips to get ready for lifelong supplementation:
Learn your individual regimen – Your bariatric team will provide specific dosages and forms of vitamins tailored to your procedure and needs. Note these down clearly.
Have supplements on hand – Stock up on a 90-day supply of your multivitamin, calcium, B12, iron, and other supplements before surgery. Continue refilling prescriptions promptly.
Organize supplements – Use a pill organizer box with compartments for each day and time supplements should be taken. This helps avoid forgotten doses.
Set reminders – Phone alerts, notes, or calendar reminders can prompt you to take supplements at the right time.
Take with food – Take vitamins and minerals with food to reduce side effects like nausea. But avoid taking iron with dairy, calcium, coffee, or tea.
Get labs done – Follow your center’s advice for regular lab work to detect potential deficiencies early.
Remember you cannot get all nutrition from food – No matter how well you eat, you likely need supplementation due to the metabolic changes from surgery.
Meet with a dietitian – A registered dietitian can help troubleshoot side effects, food intolerances impacting absorption, or low vitamin levels requiring adjustment.
Consider monthly B12 – Ask your doctor about moving from daily to monthly B12 injections for convenience and compliance.
Report issues – Notify your bariatric team if you struggle with taking supplements consistently or have ongoing side effects.
Focus on health, not hassle – View supplementation as an investment in your health rather than a burden. It is protecting you from deficiencies.
With the right mindset and preparation, lifelong vitamin supplementation does not have to be daunting. Dallas bariatric surgery centers provide the tools and support for success.
Key Micronutrients to Watch After Bariatric Surgery
While many vitamins and minerals may need supplementation, there are some that require particularly close monitoring after bariatric surgery. Being aware of these key micronutrients can help patients stay on top of their evolving nutritional needs.
Vitamin B12
Vitamin B12 deficiency is extremely common after procedures like gastric bypass and sleeve gastrectomy. This essential nutrient is absorbed in the bypassed stomach and upper small intestine. Without adequate supplementation, neuropathy, fatigue, and mental fogginess can occur.
Monthly B12 injections and high daily oral doses are standard. Levels should be monitored every 3 months initially. Some patients require ongoing adjustments to their supplementation regimen or more frequent injections to maintain optimal B12 status.
Iron
Iron deficiency is another common consequence of bariatric surgery. Women of childbearing age are especially at risk. Low iron causes anemia and impacts energy levels. Yet many patients have a hard time tolerating oral iron supplements due to constipation or stomach upset.
Working with your bariatric dietitian to find a well-absorbed iron supplement is key. Some newer forms like iron polysaccharide may be better tolerated. You may need IV iron if oral preparations remain challenging.
Calcium
Calcium deficiency can lead to bone loss and increased fracture risk after malabsorptive weight loss procedures. Ensure you meet daily calcium needs through citrated supplements spaced throughout the day. Also emphasize calcium-rich foods like yogurt, milk, kale, and sardines.
Vitamin D
Low vitamin D is common after bariatric surgery, particularly in those who lose large amounts of weight rapidly. Have your 25-hydroxyvitamin D level tested regularly, as you may need doses higher than the standard recommendation. Low D impacts bone health and immunity.
Thiamine
Thiamine (vitamin B1) deficiency can lead to serious neurological symptoms. Extended vomiting after surgery increases risk of deficiency. Be alert for signs like vision changes, confusion, loss of balance, and difficulty walking. High dose supplementation or IV thiamine may be required.
Zinc and Copper
Zinc and copper levels can drop after certain malabsorptive weight loss procedures like Roux-en-Y gastric bypass. This can negatively impact wound healing, taste perception, and immunity. Discuss monitoring and preventive supplementation with your bariatric team.
By regularly evaluating vitamin and mineral status through lab testing, bariatric teams can provide personalized supplementation regiments tailored to each patient’s evolving needs. This level of monitoring and individualization helps patients stay healthy long after surgery.
Signs and Symptoms of Vitamin and Mineral Deficiencies
Despite supplementation efforts, some bariatric patients still develop nutritional deficiencies over time. Recognizing potential signs and symptoms can help patients get timely treatment and adjustment of their vitamin regimens.
Some possible deficiency symptoms include:
- Fatigue – B12, iron, and other deficiencies can lead to tiredness, weakness, and reduced endurance.
- Hair loss – Inadequate protein, zinc, iron, or B vitamins may trigger hair loss.
- Poor wound healing – Low vitamin C, zinc, iron, and protein impair tissue repair.
- Bone pain – Can signal low calcium, vitamin D, magnesium, or phosphorus.
- Anemia – Results from iron, B12, folate, vitamin B6, or copper deficiency. Symptoms include fatigue, dizziness, and shortness of breath.
- Neuropathy – Numbness, tingling, burning, or pain in hands and feet can indicate vitamin B1, B6, B12, E, or copper deficiency.
- Night blindness – Inadequate vitamin A affects night vision.
- Confusion, memory loss – Associated with low vitamin B1, B12.
- Mood changes – Linked to vitamin D, B vitamin deficiencies.
- Skin rashes – May be seen with zinc, niacin, or vitamin C deficiency.
- Bleeding gums, bruising – Potential markers of vitamin C or K insufficiency.
- Frequent infections – Can indicate low vitamin A, B6, zinc, iron, or protein.
Don’t assume symptoms are due to other causes. Follow up promptly with your bariatric team for evaluation. Bloodwork can determine where deficiencies exist so supplementation can be adjusted appropriately. Resolving nutritional shortfalls relieves symptoms and prevents long-term effects.
Partnering With Your Bariatric Center for Ongoing Nutritional Care
Managing nutritional needs after weight loss surgery is a team effort requiring diligence from both patient and bariatric center.
Here’s how your bariatric team supports nutrition long-term:
- Provides extensive education about supplementation pre-operatively
- Prescribes appropriate vitamins/minerals post-surgery
- Orders lab work to monitor nutritional status
- Adjusts supplementation dosages and forms as needed
- Screens for and treats deficiencies
- Provides injectable options like vitamin B12 or IV iron if required
- Offers virtual or in-person dietitian follow-up
- Answers questions and helps troubleshoot issues
In turn, you play a vital role through:
- Learning about your specific nutritional regimen
- Taking supplements consistently and correctly
- Getting routine bloodwork done
- Reporting symptoms or struggles promptly
- Following dietitian recommendations
- Maintaining long-term follow-up
Together, your bariatric team and you can identify and treat deficiencies early, prevent long-term consequences, and protect your health through all the metabolic changes after surgery. Consistent vitamin and mineral supplementation along with ongoing monitoring and care are the keys to success.
Conclusion: Vitamin and Mineral Supplementation Protects Long-Term Health After Weight Loss Surgery
Bariatric procedures like gastric bypass and sleeve gastrectomy make significant alterations to digestion and absorption that increase nutritional deficiencies risk if left unsupplemented. However, with diligent vitamin and mineral replacement as directed by your bariatric center, deficiencies can be avoided.
Lifelong supplementation, along with lab work monitoring and follow-up support from your surgical team, provides the best protection against the nutritional gaps caused by weight loss surgery. Partnership between patient and bariatric center makes meeting micronutrient needs achievable long after the initial surgery. With consistent vitamin management, the benefits of weight loss surgery can be sustained while avoiding nutrition-related complications.