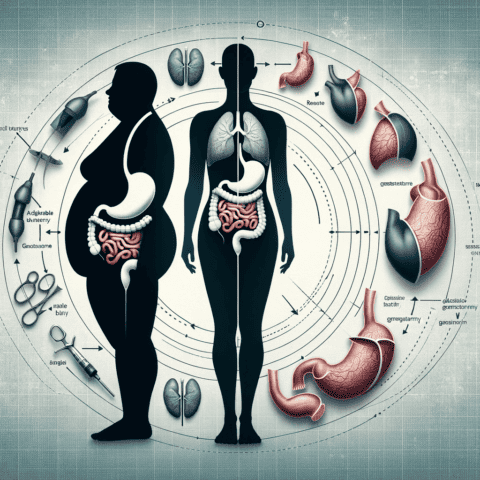
Gastric bypass is considered one of the most effective weight loss surgeries available today. In this procedure, a surgeon creates a small pouch from the stomach and connects it directly to the small intestine. This anatomy limits food intake and reduces calorie absorption from food to enable significant weight loss.
On average, those who undergo gastric bypass lose between 60-70% of their excess body weight over 12-18 months (1). For example, someone who is 100 pounds overweight can expect to lose 60-70 of those pounds and keep it off long term. Because of its dramatic weight loss impacts, gastric bypass has become the most prevalent bariatric surgery in the U.S. with over 196,000 procedures performed annually (2).
How Does Gastric Bypass Work?
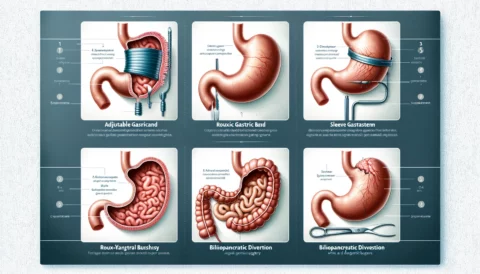
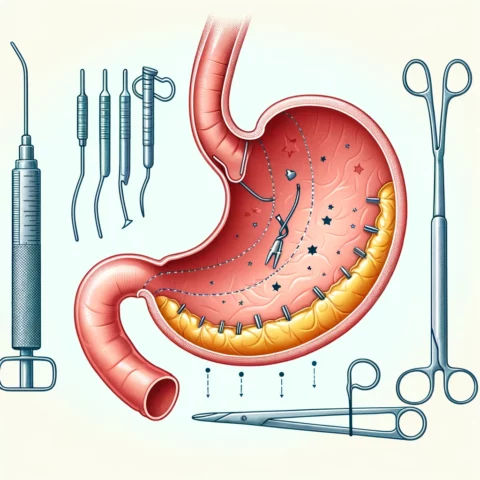
There are two main forms of gastric bypass surgery – Roux-en-Y and biliopancreatic diversion with duodenal switch (BPD/DS).
Roux-en-Y is by far the most common, accounting for 95% of surgeries (3). This procedure staples off a small section of the stomach to create a pouch no larger than an ounce. Then, the surgeon divides the small intestine and attaches the distal portion directly to the newly created stomach pouch. This rerouting process both limits how much patients can consume at one time and allows fewer calories and nutrients to be absorbed since part of the small intestine is bypassed.
The other form of gastric bypass, BPD/DS, is more complex. Along with shrinking stomach capacity, it also diverts the bile and pancreatic digestive juices that aid in breaking down fats and starches. This extended anatomical rerouting enhances weight loss but also increases malnutrition risk. Due to its complexity, BPD/DS is only utilized in about 1% of bariatric surgery cases (4).
Gastric bypass procedures can be performed as either open or laparoscopic surgeries. Open surgery involves one large stomach incision for direct access to the stomach and intestines. Laparoscopic gastric bypass uses small incisions, inserting miniaturized tools guided by a camera for improved visualization on monitors during the operation. This is a less invasive approach with faster patient recovery – most modern bypasses are done laparoscopically (5).
Why Consider Gastric Bypass? Benefits vs Risks
There are many potential benefits of gastric bypass for those struggling with extreme obesity and related health conditions:
Significant Long-Term Weight Loss
Gastric bypass enables patients to cut their food intake drastically – initially to about 1 cup volumes per meal. Combined with reduced calorie absorption from bypassing part of the small intestines, most lose over half their excess body weight and are able to sustain this loss. Studies show patients maintain 50-60% of excess weight loss more than a decade after surgery (6).
Improved Related Health Conditions
Losing significant fat mass translates to drastic improvements in medical issues driven by obesity. For example, type 2 diabetes is completely resolved in over 80% of gastric bypass patients (7). Hypertension, abnormal cholesterol levels, heart health, arthritis pain and sleep apnea also see substantial improvements for most. This reduces reliance on medications and also lowers risks for strokes, heart attacks, vascular disease and certain cancers prevalent in obese populations. Economic benefits also accrue from spending less on obesity-related healthcare (8).
Quality of Life Impacts
With substantial, maintained weight loss, most patients become more mobile and active with daily living activities. Body image and self-confidence also improve considerably. Symptoms of clinical depression frequently associated with severe obesity seem to dissipate as well. Patients report a vastly enhanced enjoyment of life after bariatric surgery outcomes take full effect (9).
However, it is vital to consider short and long-term risks before undergoing gastric bypass surgery which include:
Surgical Complications
As with any major surgery, blood clots, bleeding, infection, and other operative risks need to be taken seriously. Leaks along the staple lines created are one consideration unique to bariatric surgery that can lead to dangerous abdominal infections. Mortality risk is relatively low, however – between 0.1-2% (10).
Nutritional Deficiencies
Since the intestines crucial for absorption of vitamins, minerals and other nutrients are partially bypassed, most patients require nutritional supplements for life after surgery. Monitoring blood levels of iron, calcium, vitamins B12 and D and other micronutrients is recommended to avoid malnutrition (11).
Dumping Syndrome
Some patients experience nausea, diarrhea or vomiting after eating certain foods – especially high-calorie, high sugar options. This “dumping syndrome” results from rapid emptying of stomach pouch contents into the small intestines before food is adequately digested (12). Lifestyle adjustments are usually needed to manage symptoms.
Longer-Term Complications
Up to 20% of patients develop gallstones in their gallbladder since rapid weight loss affects bile processes and gallstone formation (13). Mild symptoms can be managed with medication but severe cases require surgical removal of gallbladder. Bowel obstructions from internal scarring or herniation may also rarely occur over time after gastric bypass.
Am I a Candidate? Preparing for Surgery
You may be eligible for gastric bypass if your:
- BMI equals or exceeds 40 (Class III obesity)
- BMI is between 35-39.9 (Class II obesity) AND you have other conditions exacerbated by excess weight like type 2 diabetes, hypertension, sleep apnea or heart disease
- Past attempts with nonsurgical methods like dieting have not achieved substantial or sustainable weight loss
Since surgery carries risks, a comprehensive health evaluation normally precedes approval for gastric bypass. This will likely include:
- Thorough examination by a multidisciplinary team – bariatric surgeon, nutrition specialist, psychologist or psychiatrist etc. (14)
- Smoking cessation
- Adjusting diet before surgery for optimal post-operative progression
- Assessing for substance abuse or mental health issues that may negatively impact outcomes
- Proactively managing conditions like nutritional deficiencies, diabetes or heart health concerns to reduce surgical risks
If gastric bypass surgery is deemed a suitable weight-loss approach for your medical needs, physical conditioning and lifestyle adjustments in the weeks before surgery can facilitate recovery.
Recovery Timeline and Long-Term Management
Patients typically stay 2-4 days in hospital after laparoscopic gastric bypass and up to a week with open surgery (15). Gradual recovery continues over 4-6 weeks at home before returning to normal activity. Managing postoperative diet and nutrition protocols is crucial – introducing foods slowly while avoiding those that aggravate side effects like dumping syndrome. Lifelong vitamin supplements and minerals will likely be prescribed to maintain your health after surgery as well.
Though recovery has its challenges, the long-term benefits make the procedure worthwhile for most patients. Expect follow-up monitoring for:
- Nutrient levels to avoid nutritional deficiencies
- Lingering conditions like high blood cholesterol or sleep apnea that may need ongoing management
- New issues like excess skin removal once major weight loss goals are met
Continuing healthy lifestyle habits also encourages long-term success. Your bariatric team will likely recommend regular exercise – about 150 minutes per week – and eating nutrient-dense, low-calorie foods about 6 times per day in small portions. Making long-term behavioral changes enhances and sustains the impacts of gastric bypass surgery (16).
Alternatives to Gastric Bypass
If gastric bypass does not seem like the right bariatric surgery option for your situation, discuss alternatives with your surgical team such as:
Sleeve Gastrectomy – Similar portion control benefits without intestinal rerouting. Reduced malnutrition risk but may have less weight loss on average (17).
Adjustable Gastric Band – Involves placing an inflatable band around the stomach versus stapling and rerouting. Less invasive procedure but also slightly less effective for weight loss based on studies (18).
Biliopancreatic Diversion with Duodenal Switch (BPD/DS) – More extreme anatomical changes for extended weight loss but higher nutritional deficiency risks (19).
Your bariatric specialists can help determine which option aligns best to your health needs and lifestyle.
Should You Consider Gastric Bypass?
For those with severe life-impacting obesity, gastric bypass surgery delivers proven and sustainable results for the majority of patients – about 60-70% excess weight loss (20). However, as a major operation it carries formidable short and long-term risks that also need proper consideration with your medical providers.
Like any medical procedure, educate yourself thoroughly on probable benefits and possible complications. Together with your healthcare team, decide if gastric bypass surgery is the most appropriate way forward for your situation. If you are deemed an eligible candidate, it could truly transform your health, mobility and enjoyment of life for years to come.