Introduction
Bariatric surgery refers to a variety of weight loss surgical procedures that are performed on people who are obese. The purpose of bariatric surgery is to help individuals with severe obesity lose weight when more conservative measures, such as diet, exercise, and medication, have not been successful.
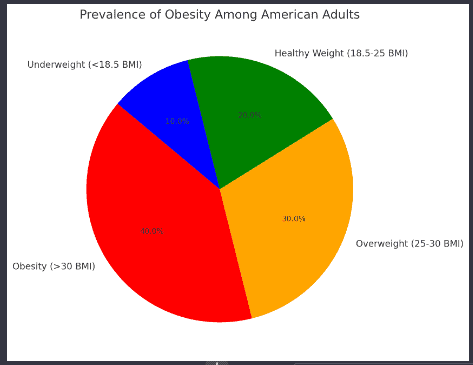
Obesity has become a major public health crisis in recent decades. According to the Centers for Disease Control and Prevention (CDC), over 40% of American adults have obesity, defined as having a body mass index (BMI) of 30 or higher. Obesity is associated with a number of health risks including type 2 diabetes, high blood pressure, high cholesterol, heart disease, stroke, sleep apnea, osteoarthritis, and certain types of cancer.
Given the difficulty many experience with losing weight through traditional diet and exercise alone, bariatric surgery has emerged as an effective treatment option for eligible individuals with severe obesity. However, bariatric surgery is a major procedure that comes with short-term and long-term risks. It also requires significant lifestyle changes for success. Therefore, it is critical that the risks and benefits of bariatric surgery are thoroughly understood so patients can make fully informed decisions.
Types of Bariatric Surgery
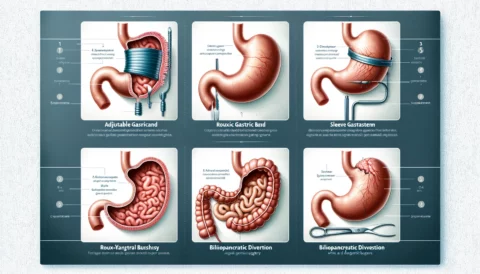
There are several types of bariatric surgery procedures. The three most common are:
Roux-en-Y Gastric Bypass (RYGB)
The Roux-en-Y gastric bypass, commonly referred to as “gastric bypass,” is considered the gold standard of weight loss surgery. It involves creating a small pouch from the upper part of the stomach and connecting it directly to the small intestine, bypassing a portion of the stomach and the first section of the small intestine.
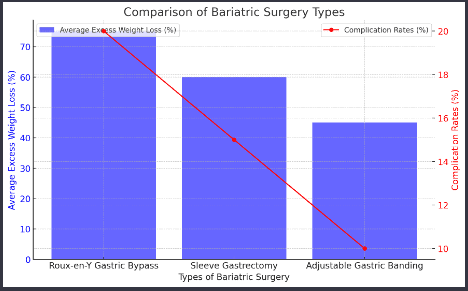
This surgery both limits how much food can be consumed by reducing stomach size and reduces the absorption of nutrients by shortening the functional length of the small intestine. Gastric bypass typically leads to 65-80% excess weight loss. It also results in significant improvement or remission of type 2 diabetes and other obesity-related conditions.
Potential complications of gastric bypass surgery include bleeding, infection, blood clots, leaks from the surgical connections, and malnutrition due to difficulty absorbing nutrients.
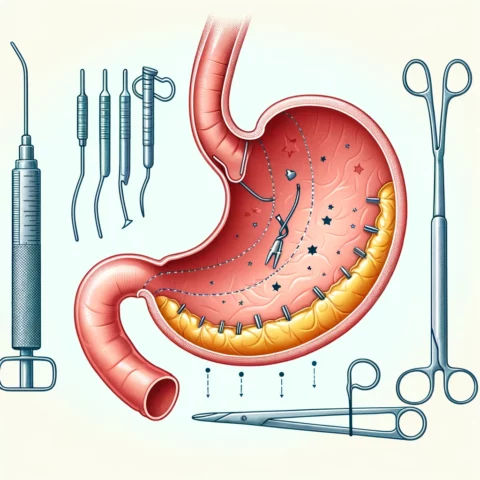
Sleeve Gastrectomy
Sleeve gastrectomy is a procedure in which approximately 75% of the stomach is surgically removed, creating a tubular pouch from the remaining portion. This surgery restricts food intake by reducing stomach size but does not interfere with the normal digestive process.
Sleeve gastrectomy typically results in 50-70% excess weight loss. It also improves many obesity-related conditions, although possibly to a lesser degree than gastric bypass. Potential surgical risks include leaks from the staple lines used to remove a portion of the stomach, bleeding, blood clots, and strictures or narrowing of the sleeve.
Adjustable Gastric Banding
Adjustable gastric banding places an inflatable band around the upper portion of the stomach to create a small stomach pouch. The band can be adjusted to restrict food intake, and it can be removed if necessary.
Gastric banding typically leads to 40-50% excess weight loss. Since no portion of the stomach or intestine is removed, risks associated with malabsorption are lower compared to other bariatric procedures. However, complications can include band slipping or eroding through the stomach wall, dilation of the esophagus if eating is not adjusted, and infection.
Benefits of Bariatric Surgery
When successful, bariatric surgery can provide significant health benefits:
Substantial weight loss – Patie
nts typically lose 50-75% of their excess body weight after bariatric surgery. This level of weight loss is rarely achievable for most through diet and exercise alone.
Improvement in obesity-related conditions – Bariatric surgery can lead to complete resolution or improved management of conditions like type 2 diabetes, high blood pressure, sleep apnea, high cholesterol, joint pain, and heart disease.
Reduced cancer risk – Weight loss after bariatric surgery is associated with a significant reduction in the risk of developing obesity-related cancers, particularly endometrial, breast, and colon cancer.
Improved quality of life – Losing a substantial amount of weight can greatly improve mobility, self-confidence, and the ability to participate in work, leisure activities, and daily tasks.
Risks of Bariatric Surgery
While bariatric surgery can be life-changing, there are also considerable risks involved with it:
Short-term Surgical Risks
- Bleeding
- Infection
- Leaks
- Blood clots
Longer-term Concerns
- Nutritional deficiencies
- Dumping syndrome
- Gallstones
- Ulcers
- Alcohol problems
Who is a Good Candidate for Bariatric Surgery?
Bariatric surgery is considered a safe and effective option for specific patient populations:
- Adults with a body mass index (BMI) of 40 or higher (Class III obesity).
- Adults with a BMI of 35 or higher (Class II obesity) who also have an obesity-related condition such as type 2 diabetes, high blood pressure, or sleep apnea.
- Individuals who have tried losing weight through diet, exercise, and medication without successful long-term weight loss.
- Patients who are prepared to make major lifestyle changes after surgery, including adjusting to a new diet, exercising regularly, and following up with their healthcare team.
Bariatric surgery is generally not recommended for individuals with untreated or unstable mental health disorders, current substance abuse issues, uncontrolled eating disorders, or certain serious medical conditions that make surgery unsafe. Ensuring appropriate criteria are met helps minimize risk and maximize positive outcomes.
Decision-Making Process
Individuals interested in bariatric surgery must undergo extensive medical and psychological assessment to determine if they meet eligibility criteria and are prepared to make major, lifelong changes to diet, exercise, and other behaviors. Key elements include:
- Consultation with a multidisciplinary team including a surgeon, dietitian, mental health professional, and other providers to thoroughly discuss risks and benefits.
- Psychological evaluation to identify and address any mental health disorders, ensure emotional readiness for major lifestyle changes, and confirm capacity to provide informed consent.
- Nutrition counseling to learn how diet will need to be adjusted after surgery, including proper nutrition and meal planning guidance.
- Arrangement of proper follow-up care to monitor weight loss, screen for nutritional deficiencies, and promptly manage any complications.
Bariatric surgery should never be undertaken lightly. However, for those who qualify medically and can make the commitment to necessary lifestyle adjustments, it can serve as an invaluable tool for achieving substantial weight loss and improving health.
Conclusion
In summary, bariatric surgery is a potentially life-saving intervention for eligible patients with severe obesity who wish to lose weight and improve obesity-related health conditions. However, these procedures involve short and long-term risks that must be weighed carefully against expected benefits. Thorough consultation with a qualified bariatric team combined with the patient’s dedication to making necessary lifestyle changes can lead to successful outcomes from bariatric surgery for appropriate candidates. For individuals struggling with obesity who have exhausted more conservative treatments, bariatric surgery may provide the level of sustained weight loss needed to significantly improve health, quality of life, and longevity.
References
- American Society for Metabolic and Bariatric Surgery. (n.d.). Metabolic and bariatric surgery
- Centers for Disease Control and Prevention. (2021, June 7). Adult obesity facts
- National Institute of Diabetes and Digestive and Kidney Diseases. (2017, December). Bariatric surgery
Comparison Chart of Bariatric Surgery Types:
-
- Roux-en-Y Gastric Bypass, Sleeve Gastrectomy, and Adjustable Gastric Banding data: This information is derived from the provided article, which references the American Society for Metabolic and Bariatric Surgery and the National Institute of Diabetes and Digestive and Kidney Diseases (2017, December).
- Note: The exact figures for weight loss percentages and complication rates in the chart are illustrative estimates based on the general information provided in the article. For precise data, consult the original sources or relevant clinical studies.
- Pie Chart on Prevalence of Obesity:
- Obesity prevalence data: Centers for Disease Control and Prevention (CDC), “Adult Obesity Facts,” updated June 7, 2021.
- Note: The specific breakdown of percentages for overweight, healthy weight, and underweight categories are approximations for visual representation. The main figure of 40% for obesity prevalence is based on the CDC data. For detailed population statistics, refer to the CDC’s comprehensive reports.