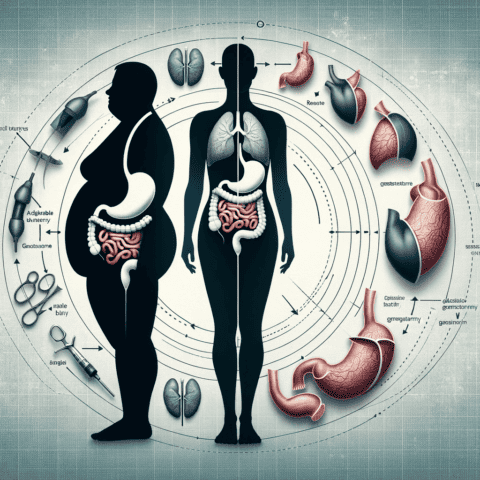
The vertical sleeve gastrectomy has rapidly become one of the most popular weight loss surgeries over the past decade. This procedure, also known as the gastric sleeve, involves surgically removing a large portion of the stomach to restrict food intake and promote weight loss. For many patients struggling with severe obesity, the vertical sleeve can be a safe, effective, and life-changing treatment option.

To better understand this transformative procedure, let’s take a closer look at what exactly the vertical sleeve gastrectomy entails.
How the Surgery Works
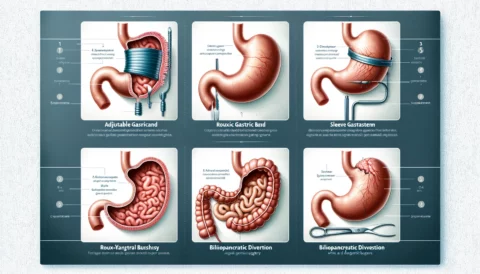
During the vertical sleeve procedure, approximately 75-80% of the stomach is permanently removed, leaving a narrow, banana-shaped “sleeve” that holds much less food. The portion of the stomach that produces the appetite-regulating hormone ghrelin is also eliminated, helping to suppress hunger. Unlike gastric bypass procedures that also reroute the digestive system, the vertical sleeve is a purely restrictive operation.
The surgery is performed laparoscopically, meaning it is minimally invasive. The surgeon operates through tiny incisions using specialized instruments and a camera. This approach typically involves less pain, lower risk, and faster recovery compared to open surgery.
Who is a Candidate?
In general, sleeve gastrectomy may be recommended for individuals with a body mass index of 40 or higher, or 35+ with obesity-related health conditions like diabetes, high blood pressure, or sleep apnea. Other factors surgeons consider include a patient’s health history, age, lifestyle habits, and personal weight loss goals. Those with inflammatory bowel disease, severe reflux, or extensive prior abdominal surgeries may not be suitable candidates.
For many patients, sleeve gastrectomy offers an appealing “middle ground” between more conservative options like diet and exercise vs more invasive surgeries like gastric bypass. However, it’s not considered suitable for those who need to lose 100 pounds or more, as the typical sleeve results in 60-80% excess weight loss.
Benefits of the Procedure
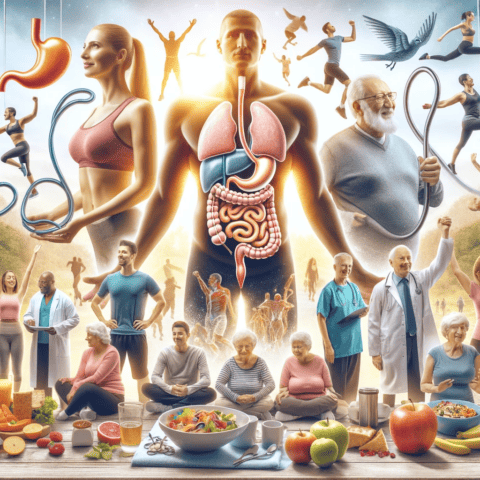
There are many potential benefits to vertical sleeve gastrectomy for qualified candidates. First and foremost, most patients experience significant weight loss of 60-70% within the first 1-2 years. This often leads to improvement or complete resolution of obesity-related conditions like diabetes, high cholesterol, hypertension, and sleep apnea (emotional journey after bariatric surgery).
Additional benefits include:
- No foreign devices or re-routing of the intestines
- Permanent removal of ghrelin-producing portion of stomach
- Higher satisfaction rates compared to lap band surgery
- No dumping syndrome side effects
- Quick recovery with no hospitalization in most cases
- Lower risk profile compared to gastric bypass
For many sleeve patients, the massive reduction of hunger and cravings makes it easier to establish healthy eating habits. However, as with any major procedure, there are also important risks and considerations.
Lifestyle Changes Needed
While the sleeve reshapes the stomach and suppresses hunger signals, the hard work of losing weight and keeping it off still requires significant lifestyle adjustments. Patients must be prepared to commit to regular exercise, nutrition planning, and portion control.
It’s also essential to work closely with your bariatric team for guidance and follow-up care. Support groups can provide an invaluable source of community and accountability. With dedication and support, the vertical sleeve gastrectomy can serve as a powerful tool to transform your health and quality of life.
Preparing for Surgery
Once you’ve decided to move forward with vertical sleeve surgery, there are important steps to take leading up to the procedure. A thorough pre-operative process helps ensure you are truly ready physically and mentally.
Consultations and Screening
The process begins with an initial consultation to review your health history and determine if you meet the basic criteria. You’ll undergo blood tests, cardiac and pulmonary evaluations, and imaging scans to screen for any issues. Psychiatric clearance is often required as well to confirm you have reasonable expectations and a support system (bariatric qualifications certifications).
Insurance Approval
Navigating insurance coverage can be challenging. Your team will help verify what your policy covers and guide you through any required pre-authorization steps. Out-of-pocket costs may range from $0 to over $20,000 depending on the provider network and benefit plan.
Pre-Op Diet
In the weeks prior to surgery, you’ll follow a strict high-protein, low-calorie pre-op diet. This kickstarts the weight loss process and helps shrink liver size for safer, easier access during surgery. Committing to the pre-op protocol demonstrates your ability to follow post-op guidelines.
Education and Support
Your bariatric program will provide nutrition and lifestyle education classes. Connecting with mentors and attending support groups can help you establish the mindset and habits needed for success after surgery.
Recovery and Aftercare
Recovery from sleeve gastrectomy is quicker than more complex surgeries, but there are still important guidelines to follow. Here’s what to expect in the days and weeks after surgery:
Hospital Stay
Most patients can go home the same day or after an overnight hospital stay. You’ll be monitored for any bleeding, leaks, or other complications. Pain is managed with IV/oral medication. Clear liquids are introduced once you are alert.
Diet Progression
Over several weeks, you’ll slowly progress from clear liquids to pureed foods to soft proteins. Taking small bites, eating slowly, and chewing thoroughly are critical to avoid discomfort, vomiting and stretching the sleeve (post-operative nutrition).
Follow-up Appointments
Frequent follow-up visits allow your bariatric team to monitor your progress, address any symptoms, and identify potential deficiencies early. Bloodwork helps ensure you are getting proper nutrition. Adjustments to medications, exercise, and eating may be needed.
Lifestyle Adjustments
Incorporating regular activity, adequate protein, and vitamin supplements lays the foundation for ongoing weight management. Support groups can help you navigate challenges, celebrations, and developing new habits (understanding the pre-surgery diet for bariatric patients).
With proper preparation and dedicated aftercare, the vertical sleeve gastrectomy offers tremendous potential to achieve significant weight loss and improve obesity-related conditions. But success requires full commitment to the comprehensive bariatric process.
Here is the conclusion for the article on vertical sleeve gastrectomy:
Long-Term Considerations
While most sleeve patients see excellent weight loss results initially, maintaining the loss involves some unique long-term considerations.
Weight Regain
It’s common to reach a weight loss plateau around the 2-year mark. Without continued adherence to proper nutrition and exercise, some weight regain is likely. Compared to bypass procedures, there is less digestive alteration to sustain very low weights.
Body Image
Massive weight loss can lead to excess skin that impacts body image and self-esteem. Plastic surgery to remove excess skin is often a later phase of the journey. Counseling and support groups can help patients adjust.
Pregnancy After Surgery
It’s recommended to avoid pregnancy for 12-18 months after surgery for safety and nutrition reasons. Working closely with your OB/GYN is essential, as sleeve patients are at higher risk for preterm birth and low birth weight babies.
Revision Procedures
Up to 20% of sleeve patients may eventually undergo a revision, or conversion to a bypass or duodenal switch if they fail to lose sufficient weight or regain most of what was lost. Revisions involve more risk and should not be taken lightly (intragastric balloon procedure).
Ongoing Medical Care
Nutritional monitoring and labwork should continue annually to check for deficiencies and ensure you are meeting protein and vitamin needs. Lifelong follow up helps detect any issues early.
Is It Right For You?
While vertical sleeve gastrectomy has many benefits, it involves permanent alteration of your digestive system. Thoroughly exploring all your options, from intensive medical weight management to endoscopic procedures, can help determine if sleeve surgery is the most appropriate choice (risks and rewards of gastric bypass).
Discussing your health history, weight goals, and motivations in depth with an experienced bariatric surgeon is invaluable. Those with chronic reflux, extensive scarring, or Crohn’s disease, for example, may be better candidates for alternate procedures.
If you decide to pursue vertical sleeve surgery, choosing a top accredited bariatric program that specializes in the procedure and provides long-term support gives you the greatest chance for success. While not an easy option, for many obese individuals sleeve gastrectomy can be life-saving and truly transformational.