Type 2 diabetes, a chronic condition that affects millions of people worldwide, is closely linked to obesity. With the increasing prevalence of obesity and its related health complications, weight loss surgery has emerged as a viable option for those seeking to improve their quality of life and manage their diabetes. In this article, we will explore the effects of weight loss surgery on type 2 diabetes and how various procedures can impact diabetes management.
Understanding the Link Between Obesity and Type 2 Diabetes
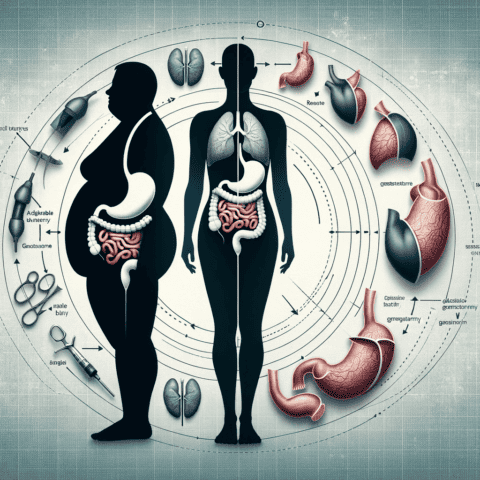
Obesity is a significant risk factor for developing type 2 diabetes, as excess weight can lead to insulin resistance. Insulin is a hormone responsible for regulating blood sugar levels, and insulin resistance occurs when the body’s cells do not respond to insulin properly. This causes blood sugar levels to rise, eventually leading to type 2 diabetes.
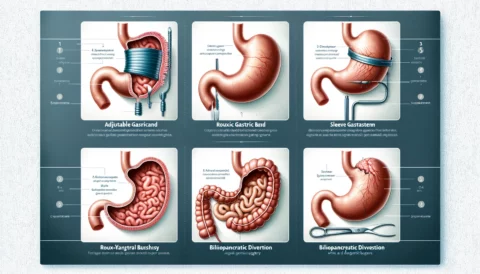
Weight loss surgery, also known as bariatric surgery, can help individuals achieve and maintain a healthier weight, thereby reducing the risk of obesity-related health conditions like type 2 diabetes. Let’s dive into the different weight loss surgery options and their effects on diabetes management.
Gastric Sleeve (Sleeve Gastrectomy)
The gastric sleeve is a popular weight loss surgery that involves removing a significant portion of the stomach, leaving a smaller, tube-like “sleeve.” This procedure limits the amount of food a person can consume, resulting in significant weight loss.
Several studies have shown that gastric sleeve surgery can have a positive impact on type 2 diabetes management. In many cases, patients experience improvements in blood sugar control, reduced dependence on diabetes medications, and even complete remission of the disease. The weight loss achieved through gastric sleeve surgery can help reduce insulin resistance and improve blood sugar regulation.

Gastric Bypass (Roux-en-Y Gastric Bypass)
Considered the “gold standard” of bariatric procedures, the gastric bypass surgery involves creating a small pouch from the stomach and rerouting the small intestine to bypass a portion of the digestive tract. This surgery not only restricts food intake but also alters the way nutrients are absorbed.
Gastric bypass has been shown to be particularly effective in improving type 2 diabetes outcomes. Many patients experience significant improvements in blood sugar control or even complete remission of the disease shortly after surgery, sometimes before any substantial weight loss occurs. The exact mechanisms behind these improvements are not fully understood, but they are thought to involve changes in gut hormones and improvements in insulin sensitivity.
Gastric Revision Surgery
Revision surgery may be an option for individuals who have not achieved their desired weight loss goals or have experienced complications after their initial weight loss surgery. Gastric revision surgery can help address issues like abdominal hernias or malnutrition and lead to improved weight loss, better blood sugar control, and an overall improved quality of life.
As with other weight loss surgeries, gastric revision surgery can improve type 2 diabetes management by promoting weight loss and improving insulin sensitivity. In some cases, patients may experience a reduction in their reliance on diabetes medications or even achieve remission of the disease.
Lap Band Surgery
The Lap Band procedure involves placing an adjustable band around the upper part of the stomach, creating a small pouch. This limits food intake and promotes weight loss. While Lap Band surgery can lead to improvements in type 2 diabetes management, it is generally considered less effective than gastric sleeve or gastric bypass surgery in this regard.
Gastric Balloon
The gastric balloon is a non-surgical weight loss procedure that involves placing an inflatable balloon inside the stomach to occupy space and reduce food intake. This temporary solution is typically removed after six months, and patients are encouraged to follow a healthy diet and exercise regimen to maintain their weight loss.
While the gastric balloon procedure may help some individuals with type 2 diabetes lose weight and improve their blood sugar control, its effects on diabetes management are generally less significant compared to more invasive bariatric surgeries like gastric sleeve or gastric bypass.
How to Choose the Right Bariatric Procedure for Type 2 Diabetes Management
Choosing the right weight loss surgery for managing type 2 diabetes is a critical decision that should be made in consultation with a qualified bariatric surgeon. Factors to consider when making this decision include:
- Your current health status and weight
- Your diabetes management goals
- The potential risks and benefits of each procedure
- Your commitment to lifestyle changes and follow-up care
A thorough evaluation by a bariatric surgeon, like those at Peak Bariatric, can help you determine which procedure is most suitable for your unique situation and help you achieve your weight loss and diabetes management goals.
The Importance of Lifestyle Changes After Weight Loss Surgery
While weight loss surgery can have a profound impact on type 2 diabetes management, it is essential to remember that these procedures are not a cure-all. Patients must commit to making lasting lifestyle changes, including adopting a healthy diet, exercising regularly, and attending follow-up appointments with their healthcare team.
A comprehensive weight loss surgery program, such as the one offered at Peak Bariatric, will include support in the form of nutrition counseling, exercise guidance, and ongoing medical care to help patients achieve and maintain their weight loss and diabetes management goals. To learn more about what to expect during the bariatric journey, visit Peak Bariatric’s comprehensive guide.
In conclusion, weight loss surgery can have a significant impact on type 2 diabetes management, with procedures like gastric sleeve and gastric bypass showing the most promising results. However, choosing the right procedure and committing to lifestyle changes are crucial for achieving and maintaining optimal health outcomes. By working closely with a qualified bariatric surgeon and a supportive healthcare team, individuals with type 2 diabetes can take control of their health and improve their quality of life.