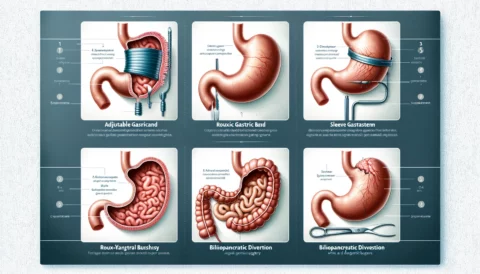
Blue Cross Blue Shield (BCBS) is a major healthcare insurance provider that offers coverage for weight loss surgery, also known as bariatric surgery. The specific requirements for coverage of bariatric surgery may vary depending on the specific BCBS plan and the individual’s location.
In general, BCBS plans typically cover bariatric surgery for people who meet certain medical criteria, such as:
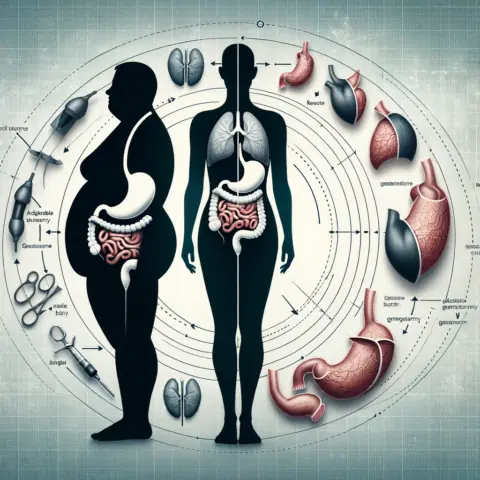
- Body mass index (BMI) of 40 or higher, or a BMI of 35 or higher with one or more obesity-related comorbidities, such as type 2 diabetes or high blood pressure.
- Documented attempts to lose weight through non-surgical means, such as diet and exercise, have been unsuccessful.
- The person is able to commit to the necessary lifestyle changes and follow-up care after the surgery.
- The person is evaluated by a team of healthcare professionals, including a surgeon and a mental health professional, who determine that the person is a good candidate for surgery.
It is important to note that these are general guidelines and the specific requirements for coverage of bariatric surgery may vary depending on the individual’s BCBS plan and location. It is recommended to contact BCBS directly or to speak with a healthcare provider to get a better understanding of the specific requirements for coverage of bariatric surgery.